Indications for surgery
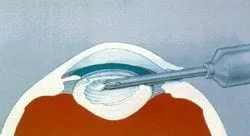
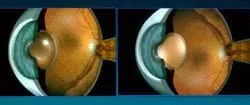
Cataracts do not have to “ripen” as they did before about 1980. Surgery before 1980 involved taking the whole cataract out in one piece and was easier to do and more likely to improve your vision if the cataract was ripe. Cataracts today are taken out in pieces and are actually easier to take out if the cataract are not ripe. Cataracts do not, with very rare exceptions, have to be taken out for medical reasons. The usual indication for removal is when the cataract decreases your vision to the point that it interferes with your daily activities and you want it taken out. Surgery is the only method available to us to remove cataracts. Until recently, we haven't used lasers to remove cataracts, but, a true laser, the femtosecond laser is being developed to remove cataracts. This new method promises to be even better than the tried and true phaco-emulsification method. ( Secondary cataracts are removed with an in office laser technique). Currently, we remove cataracts using a method called phaco-emulsification which uses a small hollow tube that oscillates back and forth very fast. This sets up waves of energy that break up the cataract into small pieces. The phaco tube then aspirates (sucks) these pieces out of the eye through its hollow middle. Phaco uses much more energy inside the eye than the older techniques, so phaco wasn’t used that much at first. When we developed intra-ocular lenses ( IOL ’s) small enough to take advantage of phaco’s smaller corneal incisions, phaco became widely accepted as the primary removal technique that it is today. Because the incisions are so small, sutures or stitches are not necessary to close the wound and this has been advertised as the no stitch method for cataract surgery.
The formal indications for cataract surgery are:
- when glasses do not improve vision enough for you to do your activities of daily living
- better visualization for the doctor to follow retinal diseases
Cataract surgery should not be done when:
- You do not want it
- the vision is not expected to improve your vision
- medical conditions exist that make cataract surgery more risky (recent heart attack, uncontrolled diabetes, recent stroke…).
- your ability to do everyday tasks are not effected by the cataract
Cataract Surgery
Surgery is performed using the phaco-emulsification method described above. In the majority of cases in the U.S., anesthesia (numbing the eye for surgery) includes using drops to numb the front and inside of the eye, to using a needle alongside or behind the eye, to general anesthesia where you are put completely to sleep. The most common method is using drops on and inside the eye, which is advertised as the no needlemethod. If you choose this method, you need to keep your eyes still during the surgery but this is not that hard to do. If you can keep your eyes still for the blue light glaucoma test during your routine eye exam, you should be OK with the drops only method. There isn’t a need for a patch after “No needle, no stitch” surgery either and you might even be able to see better on the drive home from surgery! (Someone else needs to drive you home). Needle injections alongside or behind the eye are another method. This method makes it easier for the surgeon since you cannot move your eye but does carry a higher risk of damage to the eyeball itself. General anesthesia is not used that much due to a higher risk of medical complications associated with it. (Although I remember one patient at my training program who attempted to get off the table half way through my cataract surgery. He definitely needed general anesthesia.)
Once the cataract has been taken out, it is replaced with a plastic “contact lens” whose power can be altered to compensate for you being near sighted, far sighted or having corneal astigmatism before surgery. Ophthalmologists calculate the power of this lens using the eyes length and corneal curvature. Highly near and far sighted patients need to have their lens powers fudged a little due to certain assumptions in the formula used to calculate the lens power. Today, there are even multifocal IOL’s that enable you to see up-close and far at the same time. (Just like the multifocal soft contact lenses that are available). This is why cataract surgery can be a blessing in disguise because cataract surgery can significantly decrease or eliminate your need for glasses for the distance, just like LASIK does. In fact, the optics after cataract surgery are such that the correction for near or far sightedness is optically better than it is after LASIK! This is why developing early cataracts is a contra-indication for having LASIK done. If you have early cataracts, you would be better served in the vast majority of cases by waiting a few years and having cataract surgery instead of LASIK. Having LASIK first also makes it more difficult for the doctor to measure the correct corneal curvature to determine the correct power of the IOL for your eye. Patients that cannot have LASIK due to their prescription being too high are having cataract surgery on their non-cataract eyes instead. This is called clear lens extraction. This is how successful cataract surgery has become today. I encourage all of you who have early cataracts to think about waiting and having cataract surgery instead of LASIK. If you haven’t guessed it by now, I am a fan of cataract surgery in those people who desire it and know the risks involved.
The risks include (from the American Academy of Ophthalmology pooled data):
- infection inside the eye in about 1 in a 1,000 people
- swelling in the retina (Cystoid Macular Edema or CME), significant in about 1 in 67 people
- swollen cornea in 1 in 330 people
- retinal detachment in 1 in 140 people
- need for more surgery 1 in 50 people
There are other risks as well, but these are the main ones. Certain ocular diseases can increase the risks of cataract surgery significantly higher than for the average person. Diabetics can get a lot more retinal swelling after cataract surgery and should have their retinopathy under control prior to cataract surgery. Fuch’s dystrophy not infrequently require corneal transplants after cataract surgery. Pseudo exfoliation pre-disposes to a dislocated IOL. Age-Related Macular Degeneration (ARMD) patients could have a worsening of their retinopathy but cataracts can also interfere with following the treatment of their retinas as well. ARMD patients with significant cataracts present a difficult situation for both the doctor and the patient.
Cataract surgery is rarely performed on both eyes at the same time due to the risk of infection inside the eye. As far as I am concerned, the surgeon who performs the surgery should see you themselves for the first month after the surgery. I am not a fan of optometrists following recent cataract surgery patients even if the optometrist is in the same practice as the surgeon. I have seen too many problems when an optometrist is involved during the first month after surgery. A second Ophthalmologist doing the follow-up care would be fine and probably a sign that you have a busy, successful surgeon who cared enough about you that he/she arranged appropriate follow-up care.
Bottom line: cataract surgery does involve surgery inside the eye so it shouldn’t be taken lightly, but it has improved vastly since 1980.
One last note. Unfortunately, there are aggressive cataract surgeons who push people into cataract surgery when they aren’t ready for it. Patients sometimes think that there must be a medical reason for the surgeon to want to take it out so badly and so they don’t put up much of an argument. But as I have said, taking the cataract out for medical reasons is rare and must be clearly identified ahead of time that this is the case. If you feel that you are being pushed into cataract surgery, get a second opinion. If the surgeon is badgering you, report him to the state’s medical board.
Here is the cataract surgery video that I won the 1999 national senior resident American College of Eye Surgeons (ACES) 1999 best senior resident cataract surgery award for. I got an all-expenses paid trip to go to Whistler Canada and be the guest of honor at a dinner amongst very prominent cataract surgeons and receive a $3,000 award! Being treated so nice during a residency, where you are not treated so nice, was a welcome reprieve.
(In comparing the efficiency and quality of the free charity hospital surgery center in Louisiana, where this video was shot to the private Certificate of Need/“CON” approved surgery centers here in Northern Virginia, I’ll take the charity hospital any day. The CON process is supposed to reduce the cost of surgery but instead gives the power to open a surgical center to the lobby rich hospitals which have horrendous service to ophthalmologists. The CON requirement has been fought by ophthalmologists for decades but we still have a CON requirement here in Virginia. IMHO, the CON approval requirement has resulted in much lower quality of surgery here in Virginia and is one of the main reasons why I stopped doing cataract surgery).
That said, here we go:
0:01
Corneal Incision Started. Finished at 2:26 once viscoelatic is inside the eye.
1:08
The first stab incision to enter the eye and inflate the inside of the eye with viscoelastic is performed. The viscoelastic is needed inside the eye so the eye doesn’t collapse once the bigger incision is made, which can cause all of the watery fluid inside the eye(aqueous) to rush out of the eye, collapsing the anterior chamber.
1:30
Viscoelastic is being injected into the eye.
2:26
The “big incision” entering the eye. This incision is about 3 mm in width, which allows us to inject a foldable intraocular lens (IOL) into the eye, replacing the power of the natural lens that we removed with the cataract. The IOL is about 13 mm in width including the foot pieces (called haptic). This lens is what has replaced the thick magnifying glasses that old patients were stuck with after cataract surgery 40 years ago.
3:15
The hole in the capsule surrounding the lens is performed. This is called the capsulorhexis.
4:50
Saline (salt water) is injected between the capsule and the cataract. This is done so I can manipulate the lens/cataract to aspirate (suck) it out of the eye. I will also inject saline between the cortex of the cataract and the harder center of the cataract to use the cortex as a buffer to protect the capsule from my phaco needle which you will see soon. Breaking the capsule is one of the most important goals in cataract surgery but is unavoidable in some patients. Your surgeon will probably never admit that they break the capsule but I assure you, they do.
5:30
I’m tilting the cataract on a 90 degree tilt in order to remove it more efficiently.
6:07
I am starting the removing of the cataract with a phaco emulsifying handle that uses very high frequency sound waves (not laser light, which is coming) to break up the cataract into small pieces and aspirate it out of the eye through the hole in the center of the phaco wand.
6:47
The cataract is gone, except for the remaining cortex strands.
7:23
I remove the remaining cortex with the irrigation and aspiration (I&A) tool.
10:30
I inject the thin IOL into the capsular bag that use to hold the much thicker cataract/lens. This reduction in thickness going from the lens/cataract to the thinner IOL is probably what is responsible for the attractive reduction in intra ocular pressure (IOP) that we see after cataract surgery in so many patients. This reduction is especially nice in patients with glaucoma, both narrow angle and open angle glaucoma. The dark shadowing is me trying to protect the retina from the operating light as I finish up the surgery.
This web site has taken most of its information from the American Academy of Ophthalmology’s Preferred Practice Patterns publications. Each person’s medical condition is unique and all information should be reviewed with their ophthalmologist before deciding on any course of action. We cannot be held responsible for any use, misuse or outcomes from the information contained herein. Thank you.