Age Related Macular Degeneration (ARMD)
Age related macular degeneration is a retinal disease that, unfortunately, affects our macula which is where our critical vision is. The cause of ARMD is unknown. It is thought to be a build up of metabolic waste products from the retinal photoreceptors that are normally digested by the retinal pigmented epithelium, but, for some reason, don’t get metabolized properly. 1.75 million people in the U.S. have the advanced (or wet type) form of ARMD. This is the form that frequently destroys vision. 7 million have the mild or intermediate (or dry) form of ARMD. ARMD can progress from the mild to the intermediate to the advanced form, although most people never get the advanced form. There is a pr-ARMD condition called retinal deposits. The dividing line between pre ARMD and mild ARMD seems to be the development of drusen without retinal (macular) pigmentary changes and with pigmentary changes.
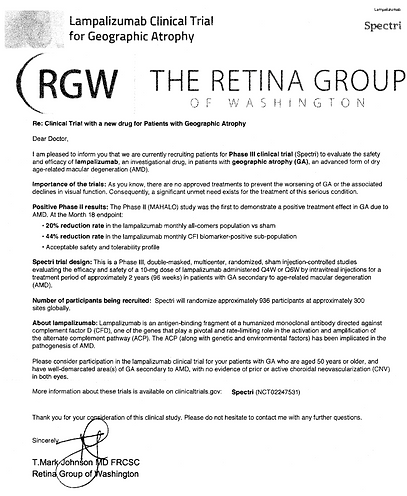
Eighty percent of people with ARMD have the non-advanced (dry) form and good vision. However, 90% of the people with "severe vision loss" (defined as legal blindness or best corrected visual acuity of 20/200 with glasses on) usually due to the advanced form of ARMD. Most of the other 10% with severe visual loss have a rare type of dry ARMD called Geographic Atrophy which is very difficult to treat. A new treatment is available with information attached below. So, most people do not have the bad type of ARMD, but those that do develop advanced ARMD have a high chance of severe visual loss. Fortunately, new medicines have, for the first time, really decreased your chances of losing vision from advanced ARMD. More on that below.
The major risk factors for developing ARMD are increasing age, smoking, Caucasian race and a positive family history of ARMD. As you can see, the only risk factor that we can control is smoking. Other possible risk factors include low blood levels of anti-oxidant vitamins and minerals.
The possibility that low blood levels of anti-oxidants and vitamin A were a risk factor for the development of ARMD gave rise to the AREDS 1 study. This study showed that certain vitamins and minerals in high doses can reduce the incidence of progressing from the intermediate to the advanced ARMD by 25% after 5 years of taking the vitamins. (Some of these people took multivitamins such as Centrum, some did not. Taking or not taking Centrum with or without the AREDS vitamins had no effect on the progression to advanced ARMD in the AREDS 1 study.) This is a lot of benefit for just taking vitamins. Omega 3 polyunsaturated fats (fish oil) may also reduce your chances of getting ARMD, as well as help your heart and your dry eyes. Be aware that if you have smoked cigarettes in the past, taking the normal AREDS 1 formula may increase your risk of developing lung cancer by almost 3-fold. Beta-carotene (a form of vitamin A) in the AREDS vitamins is the villain. If you have ever smoked, you cannot take the regular AREDS 1 formula but must instead take the formula without that form of vitamin A. (Centrum does not contain enough vitamin A to increase your chances of getting lung cancer). Zinc by itself without the other vitamins in the AREDS 1 study, reduced the chance of progressing to advanced ARMD 1 by 21% over 5 years. So, just taking the amount of zinc alone in the AREDS 1 study can significantly reduce your chances of progressing to advanced ARMD. But, zinc with the other AREDS vitamins, was even better at 25%!
The AREDS 1 study did not show a reduction in the risk of progressing from mild to intermediate ARMD for people over a five-year period of taking the high dose AREDS vitamins and minerals. It is possible that over longer periods of follow up, there may be a benefit, but for now, taking the AREDS eye vitamins is not supported by the AREDS study for mild ARMD. Only your Eye Doctor can tell you if you have the mild or the intermediate form of ARMD.
The AREDS 1 vitamin/mineral doses are as follows:
-
Beta-Carotene (A) 15 mg (25,000 IU) *
-
Vitamin C 500mg
-
Vitamin E 400 IU
-
Zinc oxide 80 mg
-
Cupric oxide 2 mg
*Some of the formulations that you buy may have slightly higher dosages due to a subsequent FDA ruling that says that labels must reflect amounts available at the end of shelf life, not the dose that was placed there when the vitamins were made.
The side effects of the high dose AREDS vitamins and minerals include; the increased risk of lung cancer (already reviewed),an increased risk of hospitalization for urinary problems (mainly in men secondary to prostate hypertrophy made worse by the zinc), and a higher incidence of the skin having a yellow tinge to it. You can have your primary care physician review your history and see if taking zinc may be appropriate for you. Remember that zinc, by itself, offers significant protection against progressing from the intermediate form of ARMD to the advanced form of ARMD. Let’s talk about Vitamin A and its cousins, lutein and zeaxanthin. Lutein and zeaxanthin are not vitamin A. They are specific types of plant micronutrients called non-provitamin A carotenoids. Both lutein and zeaxanthin belong to the broader family of organic pigments known as carotenoids. Unlike other "provitamin A" carotenoids (such as beta-carotene), lutein and zeaxanthin cannot be converted into retinol (the active form of vitamin A) in the body. While beta-carotene supports vision by acting as a vitamin A precursor, lutein and zeaxanthin have other functions. Lutein and zeaxanthin act as powerful antioxidants and light filters, concentrating in the macula and retina of the eye to protect tissues from damage caused by sunlight and free radicals.
Micronutrients
Beta carotene, lutein, and zeaxanthin are all specific types of phytochemicals (micronutrients from plants) called carotenoids, which are structurally related to vitamin A. Our bodies do not make these micronutrients; however, plants make them, in part, to serve as antioxidants* that protect them from potentially harmful sunlight. When we eat lutein and zeaxanthin, they are transported to the retina, where they are thought to protect against light-induced damage. There is normally enough lutein and zeaxanthin in the macula, the central part of the retina, to turn this part yellow. In fact, the full name of the macula is macula lutea, which means yellow spot. It has been shown that taking lutein and zeaxanthin supplements leads to increased levels of these antioxidants in the macula.
Vision Foods
Foods such as egg yolk (go easy due to cholesterol), yellow corn, orange or yellow peppers, kale, broccoli, spinach, kiwi, grapes, zucchini, and squash have high levels of lutein and/or zeaxanthin.

AREDS
For people without macular degeneration, the above foods are a good way to decrease the risk of AMD. For those with early macular degeneration, the AREDS2 vitamins are recommended. AREDS1 formula vitamins are no longer recommended as the AREDS2 formula is at least as good, and the beta carotene in AREDS1 increases the risk of lung cancer in current smokers and perhaps also in past smokers.
Family members of people with macular degeneration often ask whether they should take AREDS2 vitamins or lutein/zeaxanthin. While these are safe to take during at least five years (the duration of the AREDS2 study), it is not known whether it would be safe to take them for several decades. Therefore, it is recommended that family members eat foods containing high levels of lutein and zeaxanthin rather than take supplements. These foods also contain hundreds of other phytochemicals that are likely to be helpful.
AREDS 2
A study looking at whether different types of Carotenoids with anti-oxidants are helpful in treating ARMD. This study is known as the AREDS 2 vitamins. They include Omega 3 fatty acids, also good for your heart, Lutein and Zeaxanthin. The results have shown that the AREDS 2 study formulation was not worse than the AREDS 1 formulation in stopping progression from moderate to advanced ARMD over a 5-year period. I have decided to take one half of the recommended dosages of AREDS 2 myself. The AREDS 2 vitamins avoid the Vitamin A responsible for the increase in death associated with smokers and includes Lutein, Zinc and Omega 3 fatty acids, all common anti-oxidants. You can decide for yourself what you wish to do.
ARMD is suspected and for the most part diagnosed by your Eye Doctor when looking at your retina on a dilated eye exam. Drusen and pigment mottling are the classic appearance of ARMD as your Doctor looks at your retina. If your Eye Doctor suspects that you might have advanced (or the wet type of) ARMD, an OCT (a type of ultrasound of the retina) or a dye test called an intravenous angiogram (or IVFA) will be done. For the IVFA, the doctor will inject a dye into the veins in your arm and photograph it as it travels through your eye. Some people get a little nauseous on this test but it is a necessary test to do. Another way of detecting if you are progressing to the wet or advanced form of ARMD is through the use of the Amsler Grid. This is done by you at your home. You cover one eye, look at the center fixation dot on the grid given to you by your Eye Doctor and notice, out of the corner of your eye, if all of the lines are straight (normal), or if some of them look curved (a potential sign of developing the wet type of ARMD). Blink your eyes to make sure that debris in your tears are not distorting the grid. If some of the lines still look curved, see your ophthalmologist ASAP as this may be a sign that you might be progressing to the advanced form of ARMD. Seeing your ophthalmologist ASAP is very important as our anti-VEGF injections work better if we can start them as soon as the advanced form of ARMD begins.

Drusen, no pigmentary changes so not technically ARMD
Drusen with pigmentary changes, which constitutes dry ARMD


As discussed above, taking the AREDS eye vitamins in either the normal dose or in the smoker’s dose (which does not have vitamin A but should have zinc) can have a significant impact on your risk of developing advanced ARMD. Fortunately, if you develop the advanced form of ARMD, we have new medicines (called anti-VEGF, which stands for anti-vascular endothelial growth factor) that can arrest the neovascular growth that defines the wet type or bad type of advanced ARMD and frequently, save your vision, if we catch it in time. The FDA approved the first of these on December, 2004. These medicines are injected into the eyeball itself on a repeated basis. This may sound difficult, but many people have had this done to wonderful effect in recent years. There are some risks associated with this treatment, but I can tell you that any ophthalmologist that develops wet ARMD would want these injections done to their own eyes. Anti-VEGF treatments do not help a rare kind of advanced ARMD that does not involve neovascular growth called geographic atrophy. Aside from eye vitamins and the treatment below, not much can be done for these patients. It is a very frustrating disease for both the patient and the doctor.
As discussed above, taking the AREDS eye vitamins in either the normal dose or in the smoker’s dose (which does not have vitamin A but should have zinc) can have a significant impact on your risk of developing advanced ARMD. Fortunately, if you develop the advanced form of ARMD, we have new medicines (called anti-VEGF, which stands for anti-vascular endothelial growth factor) that can arrest the neovascular growth that defines the wet type or bad type of advanced ARMD and frequently, save your vision, if we catch it in time. The FDA approved the first of these on December, 2004. These medicines are injected into the eyeball itself on a repeated basis. This may sound difficult, but many people have had this done to wonderful effect in recent years. There are some risks associated with this treatment, but I can tell you that any ophthalmologist that develops wet ARMD would want these injections done to their own eyes. Anti-VEGF treatments do not help a rare kind of advanced ARMD that does not involve neovascular growth called geographic atrophy. Aside from eye vitamins and the treatment below, not much can be done for these patients. It is a very frustrating disease for both the patient and the doctor.
What to Know About Syfovre and Izervay for Geographic Atrophy By Reena Mukamal, Reviewed By Rahul N Khurana, MDPublished Apr. 17, 2025
Two new drugs – Syfovre (pegcetacoplan) and Izervay (avacincaptad pegol) – were approved in 2023 for geographic atrophy, a potentially debilitating type of dry age-related macular degeneration (AMD). The disease affects about one million Americans and can lead to significant vision loss.
For years, patients in the early to intermediate stages of dry AMD had a single treatment option — AREDS2 vitamins — to help reduce the risk of progression to advanced AMD. The two new drugs have heightened hope among patients and ophthalmologists alike.
“These drugs represent a scientific step in the right direction. But while these new treatments can slow down the rate of progression of geographic atrophy by a small amount, they have not been shown to have any effect on vision,” said retina specialist and Academy member Rahul N. Khurana, MD. Worse, they may cause unwanted side effects.
"It’s important to talk with your ophthalmologist about whether their benefits balanced against their treatment burden and safety risks make either of them a good fit for you,” Dr. Khurana said.
If you are considering either of these new drugs, here’s what you need to know.
How do Syfovre and Izervay work?
Geographic atrophy causes regions of cells in the retina to waste away and die resulting in a growing blind spot in the visual field. This makes it difficult to drive, read, and even recognize faces.
Syfovre (Apellis Pharmaceuticals) and Izervay (IVERIC Bio) are drugs that must be injected directly into the eye once per month, or every other month, on an ongoing basis. The drugs calm the immune response to partially prevent damage to retinal cells. The two drugs work similarly, but they target different immune molecules.
How effective are Syfovre and Izervay for geographic atrophy?
In clinical trials, patients received injections of Syfovre or Izervay monthly or every other month for one year. The drugs showed that they could slow the development of geographic atrophy by about 14% to 20%. Importantly, neither drug has demonstrated the ability to improve eyesight or restore lost vision.
These small improvements should be weighed against the burden of getting monthly injections for an indefinite amount of time – as well as the risk of side effects, some of which can be quite severe, said Dr. Khurana.
Risks and side effects of Syfovre and Izervay
Injections of Syfovre or Izervay can cause inflammation, bleeding beneath the clear lining of the eye, blurred vision, and a temporary increase in fluid pressure in the eye.
Some patients developed a separate type of macular degeneration, called wet AMD, after taking the drugs. Wet AMD can also lead to vision loss and requires treatment with eye injections of anti-VEGF medication.
Even more concerning are reports of retinal vasculitis, an inflammation that blocks blood flow to the retina and can lead to irreversible blindness. A recent report from the American Society of Retina Specialists and other industry experts described 13 patients who developed this severe complication after treatment with Syfovre, including two patients who needed to have an eye removed.
Apellis, manufacturer of Syfovre, said that the drug’s safety in the real world is similar to what was reported in the clinical trials. The company says the risk of this rare complication is very low, at 0.01% per injection.
But that may not be an accurate number, said Dr. Khurana, explaining that the people who developed retinal vasculitis did so after their first injection.
“It may be more accurate to look at [how frequently this complication happens after] first-time injections rather than among the overall number of injections,” Dr. Khurana said. In either case, “the community is concerned because the inflammation rates are higher and more severe than what we saw in clinical trials.”
Bottom line: Communicate closely with your ophthalmologist
Between heavy celebrity marketing with spokesperson Henry Winkler and the lack of any other treatment for geographic atrophy, patient interest in both Syfovre and Izervay remains high. It’s important to talk with your ophthalmologist about the risks and benefits of these drugs, based on your own personal health history.
If you are being treated with Syfovre or Izervay and experience any of the following side effects, call your ophthalmologist immediately:
-
any change in vision including blurred, wavy/distorted vision, small floating specks or flashing lights
This web site has taken most of its information from the American Academy of Ophthalmology’s Preferred Practice Patterns publications. Each person’s medical condition is unique and all information should be reviewed with their ophthalmologist before deciding on any course of action. We cannot be held responsible for any use, misuse or outcomes from the information contained herein. Thank you.
